
Anesthesia Solutions
Trust Mindray Anesthesia Solutions
Every Operating Room is different.
Choose an anesthesia machine that is tailored to your unique clinical needs.
Trust Mindray Anesthesia Solutions to build a machine personalized for your clinical needs in the OR. Our team is disrupting the industry, radically addressing today’s needs with the technology of tomorrow.
Trust Mindray Anesthesia Solutions to build a machine personalized for your clinical needs in the OR. Our team is disrupting the industry, radically addressing today’s needs with the technology of tomorrow.

Industry Leading 3-Year Warranty Coverage
Protecting your investment is important. As your trusted partner, we will assure your systems’ reliability throughout the life cycle, providing you with peace of mind. We offer an industry leading 3-year warranty on all our anesthesia systems.
Anesthesia Machines for Healthcare Professionals
Anesthesia Gas Machine
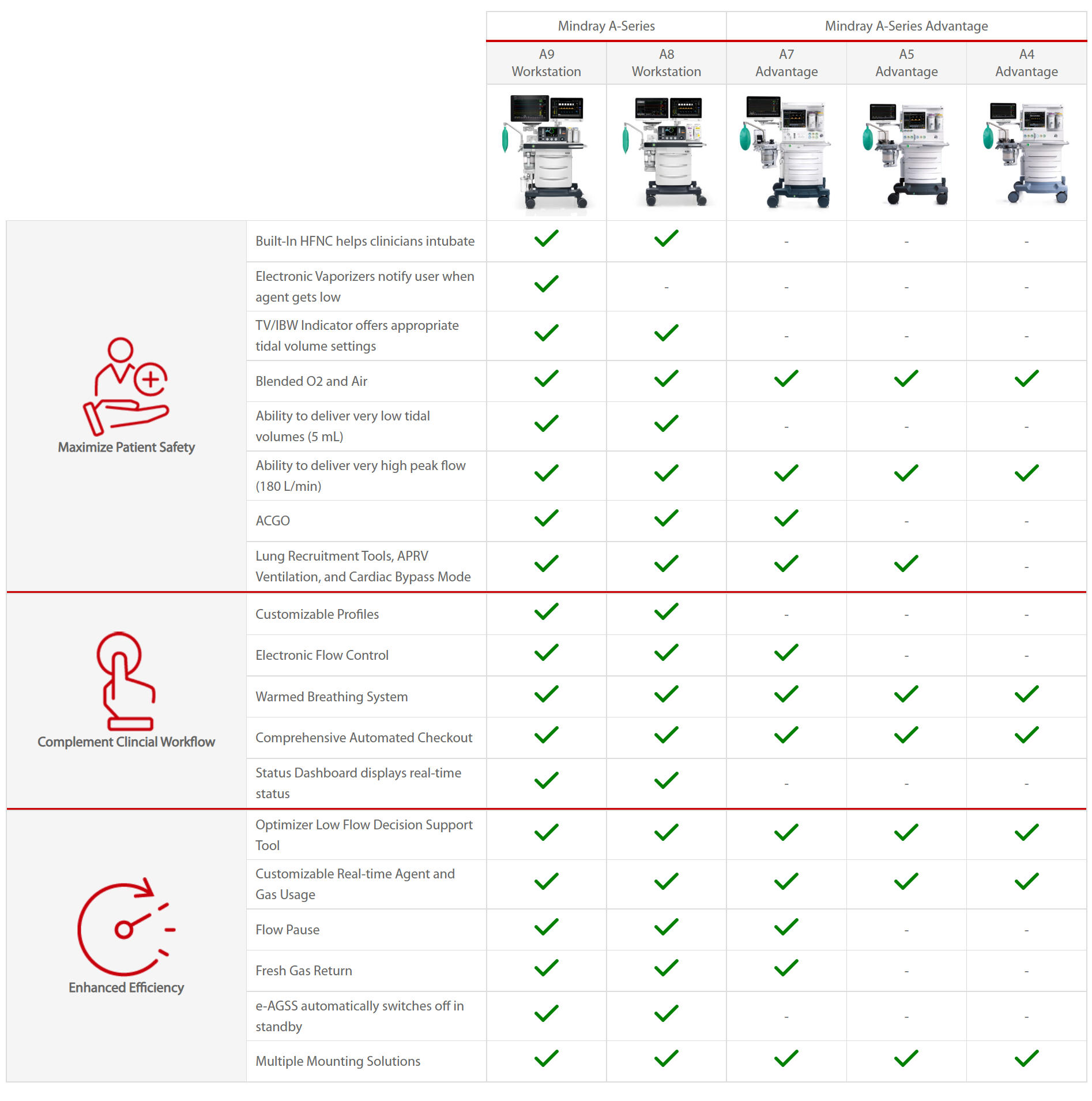
A Series Workstations
A Series Advantage
Accesssories













